Why a total hip replacement?
1. Osteoarthritis
Osteoarthritis of the hip (or coxarthrosis) corresponds to the wear and tear of the cartilage. The thickness of the cartilage surfaces decreases and exposes the underlying bone. This progressive deformation leads to a limitation of mobility, muscular aches, swelling and pain.
This joint disease is slightly more frequent in men and usually appears around the age of 60.
2. Fracture of the femoral neck
A bad fall or other trauma can cause a fracture of the femur, most frequently at the femoral neck. The risk increases sharply with age and with decreasing bone mass.
3. Aseptic osteonecrosis
It can be defined as the death of the bone cells and bone marrow of the femoral head. Necrosis is the consequence of an alteration in the blood supply to the femoral head, the causes of which are multiple (blood diseases, drugs, alcohol, medication, etc.).
It often affects a young, active adult.
4. Dysplastic hip
Dysplasias are malformations of the pelvis and/or femur. These deformities are present from birth. Unrecognised and untreated, they often lead to early osteoarthritis in the forties or fifties.
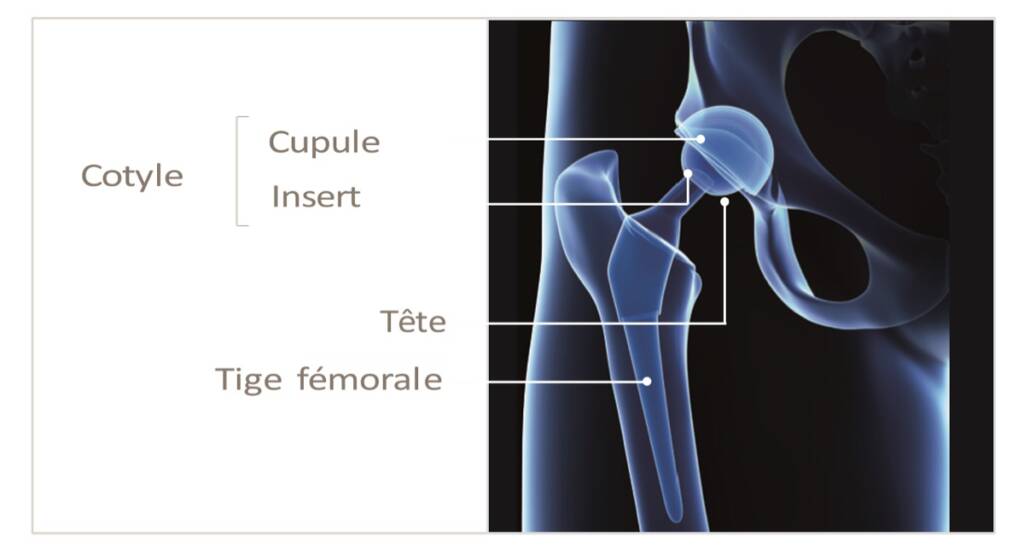
Description of the prosthesis
When the ability to walk is significantly impaired or when medical treatment can no longer control the pain, your surgeon will suggest a total hip replacement.
The total hip prosthesis is composed of a femoral stem, a spherical head and an acetabulum which is composed of a cup and an insert.
The femoral stem is generally made of metal, more precisely a biocompatible alloy of titanium for uncemented stems or of chrome-cobalt for cemented stems. The head is made of ceramic or metal.
The acetabular cup is made up of two parts, usually a titanium cup (if not cemented) and an insert, either ceramic (with a ceramic head) or polyethylene. A polyethylene cup may also be cemented, sometimes with a screwed reinforcement ring.
Description of the surgical procedure
The proposed surgery will be performed under general or local anaesthesia, as agreed with your anaesthetist.
You will be placed on the operating table, either on your back or on your side, depending on the surgical approach (anterior or posterior) used by your surgeon.
After exposing the joint, the femoral head will be resected and the acetabulum prepared for the cup and then the femoral stem.
The latter components will be implanted, with or without cement, depending on the bone quality and the operator’s practices.
This operation usually lasts between 1.5 and 2 hours, after which you will be taken to an observation unit until you recover from anaesthesia and your vital parameters are stable (usually 24 hours of observation are necessary for your safety).
Risks and complications
As a matter of principle, every operation carries general and specific risks. The surgical team strives to provide you with the best possible care to avoid any complications.
The general risks are as follows:
- Thrombo-phlebitis
- Pulmonary embolism
- Infections
- In rare cases: damage to blood vessels or nerves
The prescription of anticoagulant drugs significantly reduces the risk of phlebitis and pulmonary embolism.
Antibiotics will also be given as a preventive measure to reduce the risk of infection. However, after your discharge from the clinic, the appearance of new pain, swelling and redness in the operated area, discharge from the scar or unexplainable fever should be reported to your surgeon as soon as possible.
Pre-operative physiotherapy sessions
Some surgeons will prescribe a few sessions of physiotherapy before the operation to anticipate your apprehensions, prepare you for the use of the canes and teach you certain exercises.
However, if these sessions do not take place, do not worry, your physiotherapist will take the time to teach you the correct movements after the operation. Some technical aids may be useful.
Anticipate and familiarise yourself with this new equipment:
- Canes: these are the essential aids at the beginning of your convalescence. There are foams to place on the handles to soften the support.
- Toilet seats can be useful if your toilet is too low (or if you are tall) and you have difficulty getting up. They are available with handles.
- The wall-mounted handle for getting up from the toilet.
- The bath board: if you only have a bathtub, it can make it easier to get in. Just sit on it and swivel.
- Long tongs: can help you get dressed, pick up an object from the floor, etc.
- The long-handled shoehorn.
- Sock threader: if you have difficulty reaching your feet, it makes it easier to put on socks.
Frequent Questions
How long will I keep my two canes?
The use of the canes is usually four to six weeks depending on the surgical approach, but you should ask your surgeon how long you can use the canes.
When can I drive my car?
In general, you can drive your car as soon as you stop using the canes, i.e. 6 weeks after the operation. However, if you are using an automatic car and you have a left hip operation, your doctor may allow you to drive sooner or, depending on the type of surgery (anterior approach), this period may also be shortened.
When can I start working again? This will depend primarily on your type of activity. In the case of work requiring physical activity, the period of absence from work will be at least 2 months. In the case of sedentary work, this period could be shortened to one month and this will also depend on the surgical approach.
What about sexual relations?
This is not contraindicated. However, care should be taken with extreme movements. It is therefore recommended to remain rather passive during the first 6 weeks.
When can I take a bath?
At the beginning it is advisable to take showers standing up or sitting down using a bath board on the tub. In general, at 6 weeks, movement is free and bathing in the traditional way is allowed.
Why did my foot and hip start to swell as soon as I left the clinic?
At the clinic, your walking activity was often interspersed with bed rest with your legs elevated. As soon as you return home, you go back to your normal routine and are often standing or sitting, which encourages the migration of the haematoma caused by the operation. Remember to elevate your legs intermittently.

